known as dermatology and syphilology.
Endemic,
old-world
diseases like leishmani-
asis and garlic burns from folkloric medicine
echoed this sentiment of a traditional medi-
cal setting of a bygone era. By no means was
there a lack of technology; YAG and CO2
lasers, as well as a hair-transplant system akin
to the NeoGraft, were readily available.
A bit of pharmacotherapy culture
shock occurred as I became used to hearing
names like fusidic acid—an antibiotic used
extensively throughout the world but only
approved in 2011 in the United States after
I came back from the first trip—and various
regional preparations of betamethasone and
petroleum jelly.
Patient interaction was another platform
for learning. Every patient that walked in
was greeted with the word
salamtek
, a phrase
basically meaning “I hope you feel better.”
Jordan is considered a conservative country,
so the impression a phrase like that evokes is
only a fraction of how typical social dynam-
ics occur. Patients would often walk in wear-
ing a face veil (niqab), which I would assume
meant they must be from a very conservative
area; but in reality, they were hiding very
debilitating skin lesions.
It was a reminder that every patient
needs a clean slate in judgment despite
previous cases. A lighter tone definitely
existed, especially when elderly men figuring
that since sexually transmitted diseases were
treated here, erectile dysfunction must be
as well. After being congratulated on the
longevity of their virility, these gentlemen
5
COM Outlook . Fall 2013
s a fourth-year medical student in
2011, I had the opportunity to do
a rural selective dermatology rota-
tion in King Hussein Medical Center in Am-
man, Jordan. I knew it was going to be a great
experience when, on my first day, I walked
in on a lecture about a patient currently on
the service being treated for toxic epidermal
necrolysis. From then, it seemed a constant
kaleidoscope of skin nosology ranging from
textbook-only genodermatoses to diseases
common in the United States—but on a dif-
ferent side of the spectrum of severity.
Rather than simple mild-plaque psoria-
sis, a patient with erythroderma psoriasis
would come in, or rather than simple acne
vulgaris, a case of Morbihan disease would
present. Shingles in the United States is
the same as shingles anywhere else, but the
backdrop of a third-world country has the
effect of mystifying a disease.
Because I enjoyed my first experience
so much, I jumped at the opportunity to
visit the region again in my second year of
residency. With the nonbullous ichthyiosis
erythroderma and Netherton syndrome
cases still etched in my mind, I anticipated
what diseases I would encounter on this trip.
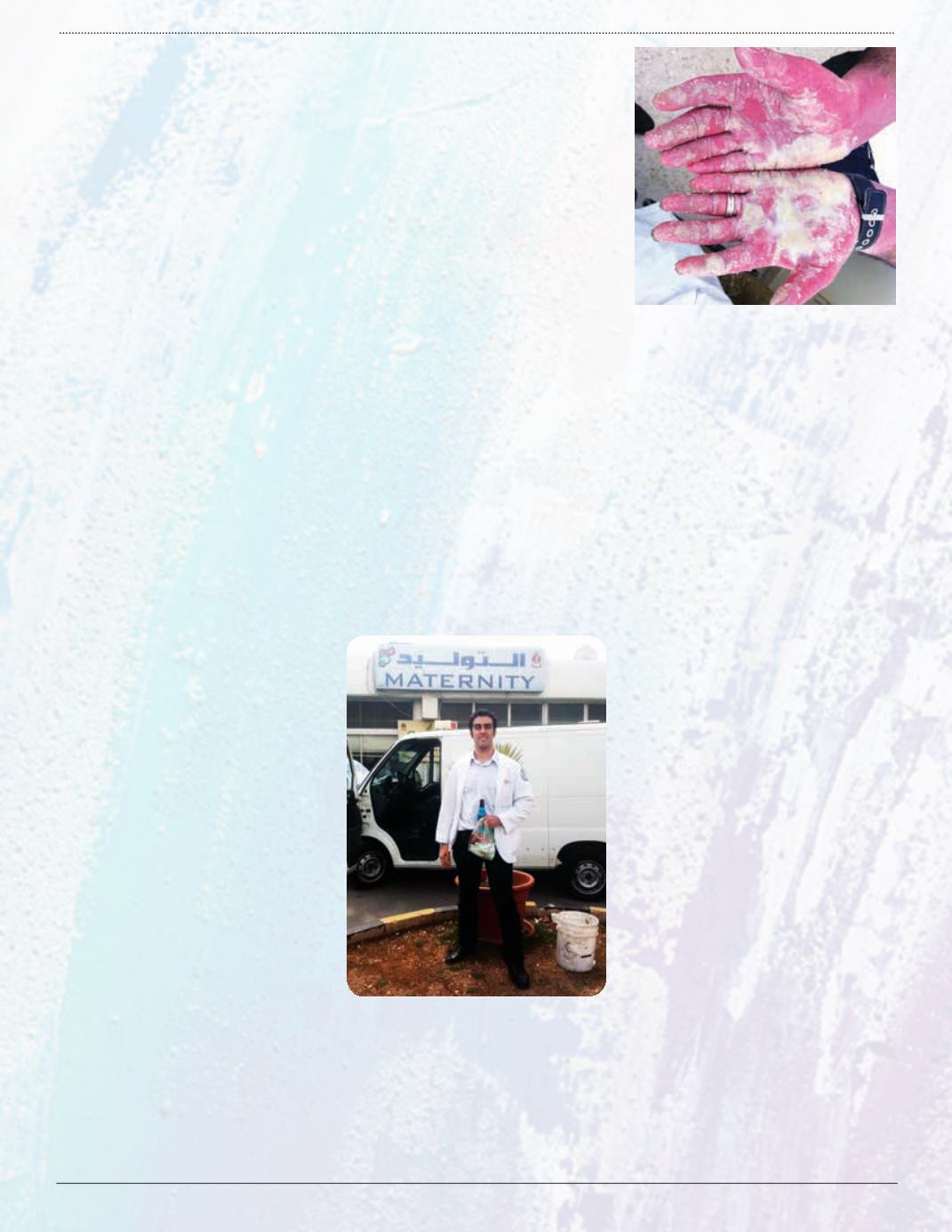
I was academically pleased with the chronic
myiasis, Vohwinkel syndrome
(pictured above
right)
, and pityriasis rotunda that could now
be added to the diseases experienced in my
career. A good case of paraneoplastic pem-
phigous or fungating psoriasis does much to
overturn old trainee complaints that derma-
tology rotations are only cosmetic or have
boring pathology. In fact, there are quite a
few dermatology-related emergencies.
In Jordan, the specialty is still known as
dermatology and venereology, much like it
was in the United States, where it was once
A
Dermatology
Rotation
Offers
Eye-Opening
Insights
By Omar Mubaidin
2011 NSU-COM Alumnus
would be politely directed to a department
that handled their complaints.
Because there was a formal Anglophone
mandate, medical education in Jordan was
taught entirely in English, so my own dif-
ficulty with Arabic was not a problem there.
Another interesting fact was how some sce-
narios of the medical education experience
do not change. Listening to the interactions
between residents and their attending was
very similar to sitting in resident lounges in
any of the South Florida teaching hospitals.
The influx of Syrian refugees provided a
new element to my residency experience. The
Zaatari refugee camp is now the second-larg-
est refugee camp in the world. With 144,000
people, this camp is now Jordan’s fourth-
largest city. I had the opportunity to go to a
primary care clinic for two days where most
of the diseases treated were rashes, upper-
respiratory infections, and diarrhea that were
more a function of living conditions associ-
ated with mass displacement.
Despite being a refugee camp, a self-
contained economy was thriving because
people had been living there for over a
year. The
main street,
which also included
field hospitals from various countries, had
butcher shops, a barber shop, a restaurant,
and a hookah lounge. Unfortunately, to go
along with the trappings of a brutal civil war,
there were stories of infiltrators trying to
poison the water system, prostitution, abuse,
and AIDS cases—an entity infrequently
encountered in that part of the world.
This was my first experience in a refugee
camp, which was more than memorable. In
fact, the entire trip of contrasts and similari-
ties in health care delivery taught me many
lessons I will hopefully carry forward for the
rest of my career.